Moving Along . . .
- Shonna L. Tropf
- Jan 16, 2019
- 16 min read
Wow, where in the heck did 2018 go? As I get older I find myself saying that quite a lot - just like my Granny said I would. (Is is much of a surprise that I did not believe her at the time?) However, like so many of you have expressed yourself, 2018 was a complete blur and gone before it seemed to even get started. I know many of my friends and acquaintances have said how they were actually more than happy to see the year be done as it was less than stellar and in some cases not even good. I would lump myself as one who was more than ready for 2018 to bid adieu.

That being said, I actually ended 2018 on a pretty positive note. My entire immediate family came out for Thanksgiving, including my oldest nephew's girlfriend, which made a total of 10 of us. We had a fantastic time. I do not take for granted for one second that my family genuinely like and love each other and actually kind of like being together! There are, after all, far too many families the cannot see past their differences to get along, let alone spend 4 days together in one house.
A few days after the family returned back to Missouri I did get very, very sick. If had I developed an incessant cough I would have sworn I had contracted RSV again as I felt that bad for about a week. (There is a previous post about my experiences with RSV. Hell. On. Earth. Period!) But, on the bright, I actually did not have much of a cough until the second week with whatever this latest round of gunk was. On the flip side of that, my chest did feel very heavy and tight. It felt like something that was not supposed to be in those airways had taken up residence and I could not convince it to move out no matter what I tried. As the cough set in my chest continued to feel even heavier/tighter and the mucus hung on. I was able to get bits and pieces up, but not enough to actually feel some relief. I'm pretty sure I may have overdosed on Mucinex during these two weeks - pills and cough syrup. I believe there was quite a bit of Tylenol, nebulizer treatments, and colloidal silver in the mix as well. I held steadfast and did not go to the doctor this time, though. Why, you ask? I can pretty much recite by heart what every doctor/nurse I would have seen would have told me and I just didn't want to hear it. I can "wait it out" on my own at home with my arsenal of respiratory remedies - I'm getting pretty dang good at using them!
Good news, I did start feeling better and was able to make the trek from CO to MO for Christmas! Lani was my super duper, reliably asleep co-pilot. Every now and again I would look back and get a one-eyed open head nod before she shifted her position and drifted back off to her doggy dreamland, which I'm sure consists of a bone-filled prairie full of mud holes and stinky things for her to role in. I actually spent two full weeks there; the longest I've been back since leaving in 2015 because of the mold exposure syndrome. I was still extremely tired and a little weak from being so sick for the previous two weeks, but overall did very well. The best part, healthwise anyway, was that I did not get sick again. Nor, and this is a BIG nor, did I contract the nasty, nasty stomach bug/flu that almost everyone around me seemed to be getting. Seriously, they were dropping like flies all around me. Fortunately this outbreak was towards the end of my trip, so I was able to escape unscathed.
It was a great trip overall! I was there long enough that I actually got to catch up with many friends and family members that I had not seen much of in the last several years. Last year I was horribly sick, so all of the plans I had made for visiting while there were squelched. This year I made up for it with a full dance card and barely had a moment of down time the entire time I was there! It was so good catching up with old friends from both high school and college. It always amazes me how we can not see each other for years at a time and then fall right back in to our friendships as if no time had passed at all. It's so nice to have friends like that.

Even though I had just seen my family a few short weeks before, we were excited to be together again and had a lovely Christmas. For various reasons, we kept things pretty simple this year and we all seemed so much less stressed over all the fuss and hub bub of the holidays than normal. I hope that's a trend we can continue in the years to come! Even with my trip being so good, I was more than ready to come home after the two weeks. I missed my bed more than anything. Lani was pretty worn out too. We've both become pretty set in our ways as we've aged and enjoy our quiet little routine in our lovely little cottage.
So now looking ahead and to get to the good TBM stuff I now you've been waiting on! 2019 has
started off pretty quietly for me thus far and I am more than thankful for that! I've been a little tired from my travels, but nothing I could not more or less push through. I did have to take one afternoon and sleep/rest, but considering where I was with my energy level, or lack there of, at this point last year I'll take it! I do have a few things coming up to look forward to in the next few months. I'll just start with what's coming up first; a consult for a bronchoscopy with my big remodel surgeon, Dr. Meguid.
Why is a bronchoscopy needed after a big remodel? For most TBM patients who've had their own remodels, also known as a tracheobronchoplasty, there is a long-term plan of care established, including regular check ups and check ins with their medical team, dynamic CT scans and possibly bronchoscopies to see if or how their TBM is progressing. Due to my being so sick this past year and being ever present at National Jewish/the ER/Urgent Care as well as my primary pulmonologist at Nat Jew and primary care physician leaving, we never really got around to fully discussing my own long-term plan of care. I suppose when you are in the pulmonologist's office every 4-7 weeks there's really no need to discuss something like that.

During a respiratory infection in October I mentioned to the nurse practitioner I saw at Nat Jew that I felt as though I needed a check in with my TBM. I told her I wasn't even sure what the proper/yearly protocol was for that. I shared with her that something felt different, especially in the area of my lungs where the smallest airways, the aveoli, were located. I told her that I was starting to hear hints of the TBM cough on occasion; nothing serious, but it was there. (Believe me that's not a cough you EVER forget once you've had/heard it.) I'm also starting to have difficulties getting secretions, aka mucus, up and out. I can feel it way down in there but if/when I finally get it worked up it's tiny specks that offer little in the way of relief. I told her I wasn't freaked out or panicked, but there was enough going on that I'd like to explore it further. TBM is, after all, a degenerative disease and I know more deterioration of the airways that cannot be supported by the magic mesh is coming at some point.
I had never seen her before and she admitted that she didn't really deal with TBM patients, but that my requests seemed reasonable and she'd check with Dr. Mohning, my new pulmonologist. She then asked what I would gain by knowing if more collapsing had occurred since there was nothing more that can be done for me. I looked at her for a minute in a bit of stunned silence until I recalled she didn't deal with TBMers (Eh, that's not uncommon!). Finding my voice, I told that I knew there was nothing more at this point in time that could be done for me, but at least I would know and the peace of mind that comes with knowing what's transpiring in my body was extremely important to me. She understood that completely.

Several weeks past and I did not hear anything, but I didn't think too much about it as fall activities and holiday decorating had begun. It wasn't until early November when I had a follow up with my sleep pulmonologist, Dr. Malich, who I really, really like by the way. (FYI: I asked why I needed multiple pulmonologists and he said Nat Jew likes to keep them separate so that if there's something going on that one of them cannot figure out then there's more heads to put together to come up with a good resolution/course of action. For the record, I have 2 pulmonologists, 1 NP I see regularly, several NPs I see when the first threes are not available, 1 neurologist, and 1 new GP.)
I had several questions for him, including what the proper " yearly check in" procedure should be for TBM patients. His primary area of focus is sleep disorders, but he does treat patients with TBM as well. He said without a doubt he recommends that his TBM patients meet with their surgeon once a year (more on this in below). He then asked why I was asking and I explained the things that I mentioned to you above. The things that struck him were the hint of the TBM cough and the fact that I was beginning to have some difficulties getting mucus up. Right then and there he put in an order for me to see Dr. Meguid.
The bronchoscopy is a scope that can go way down into my lower airways. I had several of them prior to my big remodel. I will be honest with you, I don't remember hearing too much mentioned about any collapse in my lower airways. I will have to go back in to my patient portal and review my diagnosis and doctors' notes. Having the surgeon perform the followup bronchoscopy instead of my regular pulmonologist makes it easier to spot any changes that have occurred since the big remodel.

I've sung the praises of Dr. Meguid and his magic hands many times, so I didn't mind one bit going back to him for this procedure. I saw Dr. Meguid on Tuesday, Jan. 8. He said it was great to see me, but at the same time hated seeing me because that meant I was having issues again. I dittoed his sentiments. He also said that they don't really have a yearly check in procedure unless patients are experiencing problems. So there's why I did actually have a yearly check in visit with him and I'm good with that as I see plenty of doctors as it is!I explained everything I've been dealing with both recently with TMBish symptoms as well as throughout the year plus since I'd last seen him. He was very concerned at the amount of time I've been sick and was hopeful that the surgery we were preparing for to fix my GERD will help resolve some of my continued respiratory issues and my being so prone to infections. He definitely thought we should get in there and see what, if anything, was going on with my airways and the TBM. We will proceed with a dynamic CT, which is scheduled for the 23rd. As soon as I have the CT his assistant, who will be sent the CT results as soon as they are ready, will call to schedule the bronch. He said they used to schedule both at once, but the last several they've done that has caused a lot of insurance headaches, so they schedule them separate now - gotta love insurance?
Another thing that happened recently is that I got a new pulmonologist, Dr. Stepp, yesterday. I

did not change because there were any issues with Dr. Mohning at all. I just switched to the Nat Jew clinic that is about half the distance from my house as the main campus located in downtown Denver. I first started going there to see Dr. Malich and was so excited about having to drive just 40 minutes versus well over an hour to downtown. If you're at all familiar with traffic in Denver and along Interstate 25 that runs down to Colorado Springs, then you know why this is such a good thing!

Turns out I REALLY liked Dr. Stepp, as I had been told by several folks that I would. I'd hesitated switching to the clinic for quite some time due to the fact that I was pretty attached to my NP, Katy, who is pretty amazing. However, as soon as Dr. Stepp walked into the room I immediately liked him and was made comfortable by his easy manner. He had fully reviewed my "extensive" history and issues BEFORE coming in to meet with me and was glad to see that we were being proactive with both he GERD and TBM (all kinds of acronyms and abbreviations going on in our conversation that caused some tangled tongues!). While he had me at "Hello," he sealed the deal when he said something along the lines of, " Damn, you're sick every month or so for something like a month and then sick again within a month." I saw floaty hearts swirling around his head! Oh, but then he said, "Well, obviously what we're doing is not working." Kathunk! Where had he been all my life - or at least the last year and a half?!?!
I believe that there are times when having a new pair of eyes or a fresh perspective is needed in order to truly see the whole/big picture. Dr. Stepp may just be that fresh perspective that I need. I had more or less reached the point where I was being bounced back and forth between the respiratory and GI departments on the main campus of National Jewish. No one seemed to know how to handle my case. I was repeatedly told that I was just someone who was prone to respiratory infections and that the GERD was definitely keeping my airways inflamed, making it easier for gunk to settle in. I was told that I'd just have to "wait it out," even when waiting it out stretched out for weeks and weeks and weeks. Aw, but Dr. Stepp saw my airways with new eyes and was ready to make some changes!

He said that he was sure the GI/reflux issues I have did contribute some to my respriratory issues, but that they certainly were not the cause of all of it. He said that my last set of blood tests showed some elevated numbers, nothing over the top serious, in the indicators of asthma so we should try to address those. I had previously been told those slightly elevated numbers were nothing to worry about . . . . He wondered why I was on such high doses of nubulized steroids, which are very potent in their delivery but also have a lot of particles that escape and could potentially betausinug other long-term issues such as bone lose, when I wasn't even maxed out on inhaled steroids. Hmmm, I don't know, but excellent questions!
He told me to give my nebulizer a rest, not to get rid of it, but rest it for a bit, because he wanted to changed up, not remove, the steroids I take. He bumped up my Advair to the maximum amount of 500/50 at 2 puffs/2 times a day, added another inhaled steroid, Q-Var at 2 puffs/2 times a day, and kept me on Spiriva. I am to keep my handy dandy rescue inhalers close and can use the albuterol nebulizer if I needed it. He said that changing things around was worth a shot because what we were doing definitely was not working! If it didn't work, then we'd try something new. We are keeping our fingers crossed that things will even out until my next surgery.
Which brings me to the other thing I have going on - getting my GERD fixed. I've mentioned the severity of my reflux and the issues it's caused since my big remodel. I even told you that there were several procedures that could be done to fix it. I may have even mentioned that we settled on the procedure that I am to have, but that I wasn't ready to discuss it as I had to wrestle with it, process what it was going to mean for my life, and accept all of the new changes that were heading my way.
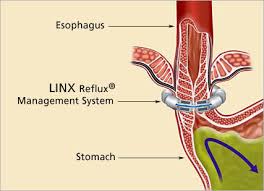
The traditional, old standard, fix for reflux is a funduplication. In recent years the Lynx procedure, which is a ring of tiny magnetic beads that incircle the esophagus, has become more popular. However, this procedure was more or less nixed right off the bat by my GI specialist, Dr. King. He said there just wasn't enough data collected on it yet and that chances of still having some reflux slip through the ring were too high for his comfort, which means it was too high for my comfort as well. (Did I mention he is ranked as one of the best GI doctors in the country and I'm lucky enough to be one of his patients!). There are a few other, lesser known and used, procedures that I won't go into.
There is one more, more invasive, procedure that's been chosen for me - a gastric bypass. Bet you didn't know that was a procedure used to fix reflux!?!? I know I did not and was a little taken aback when it was mentioned when we first realized that while the medications I was taking were helping, they were not helping nearly enough and surgery was going to be required.
When this procedure was first mentioned, by multiple doctors, as maybe being the best option for me I was so not sold on it. They all pretty much said the same things - the bypass would completely eliminate all reflux because the acid producing glands were completely sealed off from the esophagus. They would then broach my weight gain. I'm pretty candid about the weight I've gained since starting down the TBM road. In the last year and a half I've gained somewhere in the neighborhood of 30ish pounds. All of my doctors have said that a simple review of my charts shows the progression of weight gain and that they would blame the bulk of it on my being so sick and on and off of, yep you guessed it, steroids so much. For the record when it's simply mentioned that I need a dose of steroids I gain 5-7 pounds right off the bat! Their initial rationale for the gastric bypass is that I would no longer suffer from reflux AND I'd lose all of the weight I've gained and then some. We'd kill two birds with one stone. Yep . . .
It sounds easy enough, doesn't it? However, for me it was most definitely NOT that easy. During the last five years since suffering from mold exposure syndrome that ultimately lead to tracheobronchomalacia, I've given up so much of my life, or rather I've had so much of my life taken away from me. I do not have issues with food. Well, nothing that any other normal person wouldn't have during certain periods of their life when they need chocolate to get through something! I eat a relatively healthy diet, but do allow myself pizza and cookies (I really do like cookies!). I"m not a big salad eater, but I do eat plenty of veggies. Most importantly, I LOVE to cook and feed my friends and family. So in my mind I'm essentially losing everything I love about food; cooking food, trying new foods, experiencing new cultures through food, and simply bringing people together through food.

Maybe it sounds silly when one thinks of all I may gain from this next procedure. But it's not silly for me. In fact a deep seated sadness settled in and stayed put for a few weeks. I tried to force it down and away, but it was stubborn in its steadfastness. This surgery was never ever in my prevue of something that I'd need. I've always been a little chunky; I am built just like three of my great grandmothers so my body shape was a foregone conclusion before I ever actually came into being. However, I've been healthy and active so being a little fluffy was just part of who I was. For the record I've always weighed more than people thought because there was a lot of muscle under the fluff! :)
I even kept the fact that I had to have this particular procedure to myself (I did share I with my family as well.) for several weeks. Not because I was embarrassed or ashamed in any way of having to have it, but because I just could not wrap my head around it, around yet again having to lose another part of my life to these diseases/conditions I've found myself with. One of my sweet guy friends got a little riled up when I revealed I would be having this procedure and my feelings about it. He was very forceful in reassuring me that I should not worry about what others thought or any social stigmas about this surgery because they were stupid anyway. He didn't stop there! He said I'd been sick and that anyone who knew me knew how

active I liked being - and my calves and legs were the proof of that. Aaawwww shucks! (He's
right, even after being so sick and not as active as I want to be this past year, my calves are still rock solid!) After explaining that I didn't care one iota about what people thought or social stigmas, but it was more about my own losses thus far and the future losses this procedure would bring made him step back and actually get my point of view. However, it's reactions like his and so many of my friends/family that make me realize just how fortunate I am to have such a good support system in place.
Meeting with the surgeon to go over my options is what finally made me begrudgingly accept my fate and realize that a gastric bypass was definitely in my future. She was very personable and I was immediately comfortable with her. She was extremely thorough in her explanations of each procedure - and why they were not options for me. Then we get to the bypass and she tells me this is my only option, no ifs ands or buts. With my weight gain and all of the other comorbidities that I have the other procedures just would not be effective in the long term and that I would most likely end up with reflux issues in the future. To her that was not acceptable, so to me that was not acceptable. She assured me that the bypass would completely do away with the reflux. The only concern she had was that due to my having to be on steroids so often that perhaps an ulcer may form at the incision cite from the acid hitting it. Her fix would be to have me take one antacid type pill a day as a preventative measure, which is so much better than the seven I take now!
So, all in all things are moving along. I've started the process of required meetings with the dietician, psychiatrist, the surgeon's nurse practitioner, and more meetings with the nutritionist. I only have a couple of more meetings to go before having the procedure. We are hoping to have it done by the end of February or first part of March, which will be here before we know it! I will keep you all posted as things progress and as we get a surgery date in place. That's enough for now. As always, thank you so much for sharing in my journey with me. Wishing you the blessings of mercy and grace in your own journey, whatever that may be.
Shonna



Comments