Tracheobronchoplasty
- Shonna L. Tropf
- Aug 22, 2017
- 6 min read
Update #4 8/22/17
Warning: I will be discussing the tracheobronchoplasty in detail. If you have a queasy tummy, you may want to skip this one. . .
My big remodel surgery was originally scheduled for August 31. However, due to my surgeon having a family emergency that took him to Florida to be with his father this past week it has been pushed back until September 7, only a week later. The reason for this is that most of the surgeries he had to reschedule were lung cancer patients, so they definitely take precedence – as they should.
Several people have inquired as to what exactly the big remodel will entail. It’s a doozy! Tracheobronchoplasty is the official name for the procedure. The procedure starts with an 8” – 10” incision on my upper right side/back just under/along side my breast area. Well technically I will be administered anesthesia and sent off to dreamland first and thank goodness for that! Next, Dr. Meguid will remove one of my ribs, gulp!
Just a quick aside, I had read several articles on this procedure and pretty much knew what I was in for – except for the rib removal part. I must have scrunched up my face and I know I withdrew further into the corner of my chair, because the doctor started laughing and said, “What’s that look for? You don’t need that rib and I need it out because I have to get my hands in there!” Right he is. . . So, I’m going to lose a rib. God took one from Adam to create Eve. Dr. Meguid is going to take one from me to give me breath and my life back. It’s a fair trade.
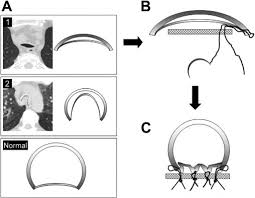
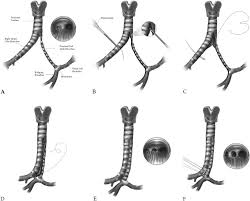
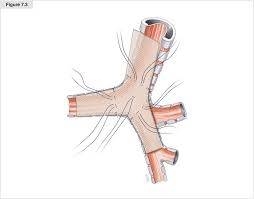
The next phase of the tracheobronchplasty is to lift my trachea up and away from the chest cavity and measure it for the knitted polypropylene mesh that will be stitched to the complete underside of the trachea and down into the bronchi until they become a full cylindrical shape as they begin entering the lungs. The mesh will be attached using polypropylene threading with rows of four sutures placed across trachea every 5-7 mm (see link 1). Rows of sutures will continue until the bronchi become smaller and will then become rows of three sutures.
I did ask my surgeon if there was a robotic arm or if it was he who would be doing the stitching. He emphatically stated it was all him and held up his hands, wiggling his fingers for me to get a good look at. He said there’s no room for such robotics in this particularly delicate procedure and that he had to be able to feel his way through it. Dr. Meguid then went on to tell me who all would be in the operating room with us and what they would be doing. He said his assistant would help with the suturing at times, but assured me his assistant was every bit as good as he was or he would not be in the OR with him. Good to know!
The purpose of the mesh is to pull the collapsed, or malacic, portion of the trachea down in order to hold it open so that air passes unimpeded through the airways all the way down into my lungs. The mesh and sutures are permanent, as is the rib removal. Eventually scar tissue with begin to grow over the mesh and sutures, securing them in place for the rest of my life – barring any complications, which are rather rare, that is.
The images on the bottom row are a bit graphic. Feel free to skip!
Once the tracheobronchoplasty is finished, which should take 4 - 6 hours (Dr. Meguid said 4, everything else I've read and talked to, including the nurse said more like 6. He's optimistic!), they will stitch me up, leaving two drainage tubes in the incision and wheel me to the ICU, where I will stay for 1 - 4 days Everything I've read says something a little different on the ICU stay. I won't be left to just lay around, though. I will be up and walking that first day. To quote Dr. Meguid, "You will be in a severe amount of pain, but you have to get up and walk, whether you want to or not." I assure you all, that I will do whatever I have to in order to get better and I will walk through the pain! I may have a few choice words and a LOT of prayers to say at the time, but I will get through it. He also told me I would be going through intensive respiratory therapies the entire time I"m in the hospital, which is a week to nine days, again depending on what I read. Additionally, I will continue with the respiratory therapies once I am allowed to go home. All of the walking and therapies is to aid in recovery and to help stave off infections and possible complications.
Full recovery time for this procedure is 6 - 9 months. At four weeks we may consider me going back to work part time. However, Dr. Meguid, not to mention my boss Tim, said he would ere on the side of my recovery and he would not push it. At six weeks I should be at about 85% and may be able to go back to work, which considering I don't remember the last time I was at 85% full-health I should be more than good to go! Oh, but then there's Dr. Meguid, who once again said he would ere on the side of my recovery and would not release me to go back to work if he did not feel I was ready, and again Tim concurred. I will abide, however begrudgingly, with whatever he tells me, because in all seriousness, I do not want to do any harm/damage to my airways by being over zealous with my recovery and pushing myself too hard too fast (I just so happen to be an expert at that, but I'm working on it!).
So, the possible complications is a fairly lengthy list. I will just go through the big ones for you. Dr. Meguid did go through all of them and provided the statistics for each one, so I'm well prepared for anything that most likely will not happen. The biggest fear is pneumonia, hence the immediate walking. The stats on acquiring pneumonia after this procedure were actually pretty high, but I am in excellent hands and am not too worried about that. Infections of any kind, whether at the incision site or in my airways are also of big concern. The list goes on and on from there, but you get the gist.
Managing my "severe" pain, mainly due to that dang rib removal, is something else that will be monitored around the clock. I will have the handy dandy, magic button again and even more pills regularly administered by the nurses. I was already sent home with a hefty amount of pain meds after the stint trial. I could totally make some serious bank on the black market with that stuff - I am totally just kidding, but seriously I could! :) Between the amount of anesthesia I'll be given while being under 4 - 6 hours and that pain meds, I will be all kinds of loopy for sure! Did I tell you that last week I somehow managed to drop my work name tag in the pot boiling water as I made Lani's food (yes, I make her food due to her food allergies). No idea - at all - how that happened. No recall of it whatsoever, but I did it. It makes for a great conversation piece at work, though! :)
Below I have provided a few of the ever so stimulating articles I read to prepare myself. In all honestly, because this is happening to me, I did find them to be very informative and helpful. Because they are grounded in science and research, they took away some of the emotions and anxiety connected to something this major. I am thankful for my training as a researcher so that I knew how and where to search for this type of information and that I was able to understand what I was reading (for the most part - I did have to look up a few key terms, though!).
Whew, I think that's enough for today. Please do not hesitate to contact me if you have any additional questions or if you just want to talk. I'd love to hear from all of you. Thank you again for your good juju thoughts and prayers. I cannot express how much they mean to me as I move through this journey. Blessings!
Sources and Resources:
http://www.annalsthoracicsurgery.org/article/S0003-4975(11)00023-3/pdf
2. http://www.jtcvsonline.org/article/S0022-5223(12)00564-8/fulltext
3. http://www.sciencedirect.com/sdfe/pdf/download/eid/1-s2.0-
S1053077016306322/first-page-pdf
4. http://www.annalsthoracicsurgery.org/article/S0003-4975(11)00023-3/pdf
Oh, here's the link to my gofundme page!
https://www.gofundme.com/shonnastbmremodel

Comments